Essential Root Canal Pain Management Information
- Root canal therapy preserves your natural tooth while eliminating infection
- Most patients experience minimal pain during the procedure thanks to effective local anesthesia
- Post-treatment discomfort is normal but typically subsides within a few days
- Over-the-counter medications and cold compresses are usually sufficient for pain management
- Proper aftercare including soft foods and good oral hygiene speeds recovery
- Modern endodontic techniques have made root canals more comfortable than ever before
- Approximately 95% of patients experience successful outcomes with appropriate pain management
- Pre-treatment anxiety can be effectively managed with various sedation options
- Most root canal procedures can be completed in 1-2 appointments
- Follow-up care with your dentist ensures long-term success of the treatment
If you’ve been told you need a root canal, you might feel anxious about potential pain during and after the procedure. The good news is that modern dentistry has made tremendous advances in pain management techniques for endodontic procedures. Today’s root canal treatments are far more comfortable than their reputation suggests, with many patients comparing the experience to receiving a routine filling. Advanced anesthetics, precision instruments, and improved techniques have transformed what was once a dreaded procedure into a relatively comfortable experience with predictable outcomes. In this comprehensive guide, we’ll explore the various options available to manage discomfort throughout the root canal process, from pre-treatment preparation to post-procedure recovery. Understanding these pain management strategies can help alleviate anxiety and ensure a more positive dental experience.
What is Root Canal Therapy?
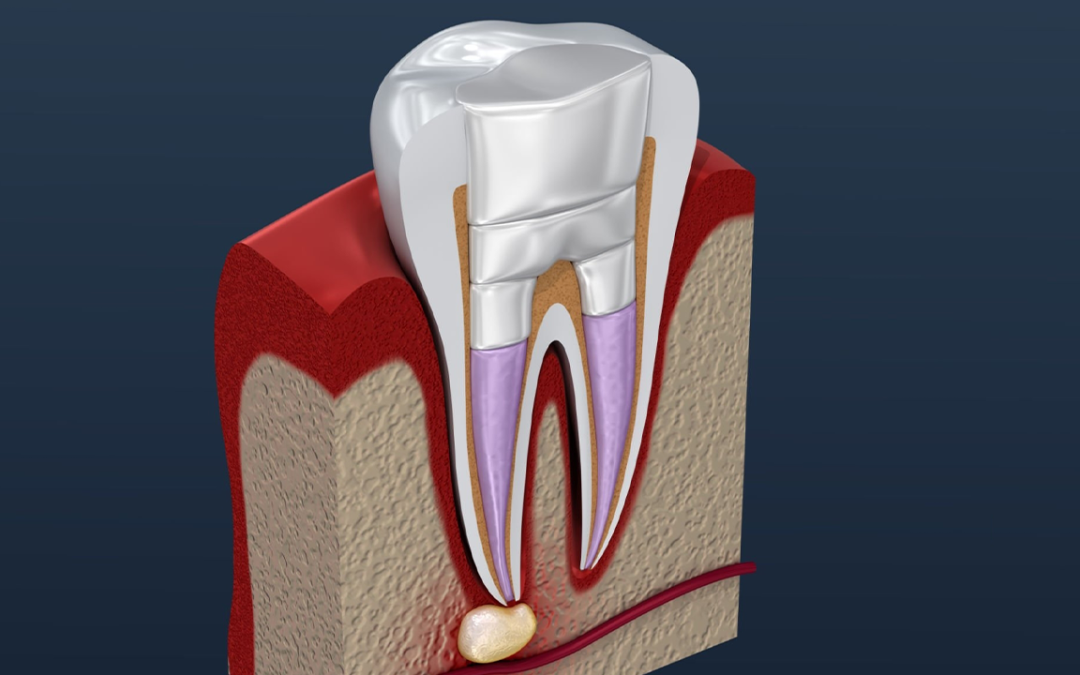
Root canal therapy, also known as endodontic treatment, is a dental procedure designed to save a tooth that has become infected or severely damaged. When the soft inner tissue of a tooth (the pulp) becomes infected due to deep decay, repeated dental procedures, cracks, or trauma, a root canal becomes necessary to prevent the spread of infection and save the natural tooth. This specialized procedure addresses problems affecting the tooth’s nerve and blood vessels, which are housed within small, narrow passageways (canals) that extend from the central pulp chamber to the tip of the tooth’s roots.
During the procedure, the infected or damaged pulp is carefully removed, and the inside of the root canal is cleaned, shaped, and disinfected. The endodontist uses specialized instruments to access and thoroughly clean these microscopic spaces, removing all traces of bacteria and infected tissue. The space is then filled with a biocompatible material called gutta-percha and sealed to prevent reinfection. In most cases, a crown is later placed on the tooth to protect it and restore full function. This final restoration is crucial as it protects the treated tooth from fracturing and restores its ability to withstand normal chewing forces.
Many people associate root canals with pain, but the reality is that the procedure is performed to relieve pain caused by infection or inflammation, not create it. With proper specialist dental care, most patients experience little to no discomfort during the procedure and are surprised by how straightforward the process actually is. Modern endodontic techniques, including digital imaging, operating microscopes, and specialized instruments, have dramatically improved the precision and comfort of root canal therapy. Statistics show that root canals have a success rate of approximately 95%, making them an excellent option for saving natural teeth that might otherwise require extraction.
Common Causes of Root Canal Pain
Understanding the sources of root canal pain helps patients recognize when they might need treatment and what to expect during recovery. The primary cause of pain before a root canal is infection and inflammation of the dental pulp. When bacteria invade the pulp chamber through deep cavities, cracks, or leaky fillings, they cause the pulp tissue to become inflamed and infected. This inflammation creates pressure within the confined space of the tooth, leading to significant pain that may radiate to the jaw, face, or other teeth. The immune system’s response to bacterial invasion further intensifies this inflammation, causing increased blood flow to the area and additional pressure on the nerve endings within the pulp.
Nerve damage is another common source of pain. The dental pulp contains nerves that, when damaged or irritated, send pain signals to the brain. This damage can result from trauma, extensive decay, or even the pressure from a growing infection. The nerves within the dental pulp are particularly sensitive to both pressure and inflammatory chemicals released during infection, which explains why pulpal inflammation can cause such intense discomfort. In some cases, the pain you experience may not be coming directly from the affected tooth. This referred pain can make it difficult to identify which tooth is actually causing the problem, which is why professional diagnosis by an experienced endodontist is crucial before proceeding with any treatment.
After a root canal procedure, some temporary sensitivity or discomfort is normal as the tissues around the tooth heal. This is typically mild and can be managed with appropriate pain management strategies. It’s important to remember that this post-treatment discomfort is part of the healing process and usually subsides within a few days. The source of this discomfort is often inflammation of the periodontal ligament that surrounds the tooth root, rather than the tooth itself, since the nerve has been removed during treatment. Occasionally, patients may experience what feels like pressure or a dull ache as the body’s inflammatory response continues during the healing phase. This is a normal part of recovery and typically resolves as inflammation subsides.
Pain Management Before Root Canal Treatment
Managing pain before your root canal procedure can help ensure a more comfortable experience. If you’re experiencing pain while waiting for your appointment, there are several strategies that can help provide relief. Over-the-counter pain medications such as ibuprofen (Advil, Motrin) or acetaminophen (Tylenol) can help reduce pain and inflammation. For many patients, a combination of ibuprofen (600mg) and acetaminophen (500mg) taken every 6 hours can provide effective relief without the need for prescription medications. This combination approach targets pain through different mechanisms simultaneously, offering more comprehensive pain control than either medication alone.
Avoiding hot and cold foods and beverages can also help minimize pain, as temperature extremes can trigger sensitivity in an infected tooth. Sticking to soft, room-temperature foods puts less pressure on the affected tooth and can reduce discomfort. Dental researchers have found that thermal stimuli can cause rapid fluid movement within the dentinal tubules, which directly stimulates nerve fibers and causes pain in compromised teeth. Some patients find relief by applying a cold compress to the outside of their cheek near the painful tooth. This can help reduce inflammation and temporarily numb the area. Apply the compress for 20 minutes, then remove it for 20 minutes, repeating as needed. The cold temperature constricts blood vessels, which reduces blood flow to the area and helps minimize swelling and pain.
If your pain is severe, contact your general dentist or endodontist right away. They may be able to prescribe stronger pain medication or antibiotics if an infection is present. In cases of acute infection, antibiotics may be necessary to control bacterial spread before the root canal procedure can be performed safely and comfortably. Remember that these measures provide temporary relief – the root canal procedure itself is necessary to address the underlying cause of your pain and prevent further complications. Many dental practices now offer emergency appointments specifically for patients experiencing severe dental pain, as prompt intervention can significantly improve comfort and treatment outcomes.
Pain Management During Root Canal Treatment
One of the most common concerns patients have about root canal therapy is pain during the procedure. Modern dentistry has made significant advancements in pain management, making root canals much more comfortable than they once were. The primary method of pain control during root canal treatment is local anesthesia. Before beginning the procedure, your dentist will carefully administer anesthetic to numb the tooth and surrounding tissues completely. Many patients report feeling pressure during the procedure but no pain. Today’s anesthetics are more potent and longer-lasting than earlier formulations, and dentists often use computer-controlled delivery systems that provide more comfortable and effective numbing.
For patients with dental anxiety or those undergoing complex procedures, various sedation options are available. Nitrous oxide (laughing gas) provides mild sedation that helps you relax while remaining conscious. This safe, effective gas is administered through a comfortable nose mask and wears off quickly after treatment. Oral sedation involves taking medication before your appointment to induce a deeper state of relaxation. This approach is ideal for patients with moderate anxiety and allows you to remain awake but deeply relaxed during treatment. For maximum comfort, IV sedation puts you in a deeply relaxed state while maintaining consciousness. Your dental professional will discuss which option is most appropriate for your specific needs and medical history.
Our practice utilizes state-of-the-art equipment and techniques to make your root canal treatment as efficient and comfortable as possible. Digital imaging allows for precise treatment planning, while rotary instruments help complete the procedure more quickly and with less discomfort than traditional hand files. Operating microscopes provide enhanced visualization of the tiny root canal spaces, allowing for more thorough cleaning and less trauma to surrounding tissues. Throughout the procedure, your dentist will check in regularly to ensure you’re comfortable and provide additional anesthesia if needed. Many endodontists also employ techniques like buffered anesthetics (which are less painful to administer) and supplemental injection techniques to ensure profound anesthesia even in difficult-to-numb situations, such as teeth with acute infections.
Post-Root Canal Pain Management Strategies
After your root canal procedure, some discomfort is normal as the area heals. This typically subsides within a few days and can be managed with various strategies. For most patients, over-the-counter pain relievers are sufficient to manage post-treatment discomfort. Ibuprofen (Advil, Motrin) reduces inflammation and pain, while acetaminophen (Tylenol) provides pain relief without anti-inflammatory effects. Naproxen (Aleve) offers longer-lasting pain relief. Our dental team will provide specific recommendations based on your medical history and the complexity of your procedure. Clinical studies have shown that taking pain medication preemptively (before pain develops) and on a regular schedule for the first 24-48 hours is more effective than waiting until discomfort becomes severe.
Applying a cold compress to the outside of your face near the treated area can help reduce swelling and numb the area. Apply the compress for 20 minutes, then remove it for 20 minutes, repeating as needed during the first 24 hours after treatment. This approach helps constrict blood vessels and limit inflammatory mediators to the area, reducing both swelling and discomfort. Beginning 24 hours after your procedure, gentle saltwater rinses can help keep the area clean and promote healing. Mix half a teaspoon of salt in 8 ounces of warm water and rinse carefully. The saltwater solution creates an osmotic gradient that draws out fluid from inflamed tissues while providing a mild antimicrobial effect.
While your mouth is healing, it’s best to stick to soft foods that require minimal chewing. Our dental surgery recovery guide offers excellent suggestions for post-procedure nutrition. Avoid extremely hot, cold, or spicy foods that might irritate the treated area. Getting adequate rest with your head slightly elevated can help reduce swelling and discomfort. Try to avoid strenuous activities for at least 24 hours after your procedure. Research indicates that elevated heart rate and blood pressure from exercise can increase post-operative discomfort by increasing blood flow to inflamed tissues. Most patients find that discomfort peaks within the first 24-48 hours after treatment and then gradually subsides. By following these recommendations and maintaining good oral hygiene (while being gentle around the treated tooth), you can support faster healing and minimize discomfort.
When to Contact Your Dentist About Root Canal Pain
While some discomfort after a root canal is normal, certain symptoms may indicate a problem that requires professional attention. Contact your dentist immediately if you experience severe pain that doesn’t respond to prescribed medications, significant swelling that worsens after 2-3 days, or an allergic reaction to medications. These symptoms could indicate a persistent infection or an adverse reaction that requires prompt intervention. You should also seek care if you notice the return of symptoms that were present before the root canal, loss of the temporary filling or crown, visible swelling inside or outside the mouth, or fever, which may indicate infection. Endodontic research shows that approximately 3-6% of root canal treatments may require additional intervention, so it’s important to report concerning symptoms promptly.
It’s important to remember that most patients experience a gradual reduction in discomfort over the first few days following treatment. By the third or fourth day, pain should be minimal or absent. If your pain is increasing rather than decreasing, or if it suddenly returns after a period of improvement, these could be signs that something isn’t healing properly. Persistent bite sensitivity that doesn’t improve after a week may indicate that the tooth restoration needs adjustment. Our dental surgery specialists are available to address any concerns that arise during your recovery. Many practices now offer virtual consultations for post-operative questions, allowing you to discuss concerns without necessarily coming into the office.
Regular follow-up appointments are essential to monitor healing and ensure the success of your root canal treatment. If your tooth was fitted with a temporary filling, you’ll need to return for a permanent restoration, typically a crown, to protect the tooth long-term. These appointments are an important part of the treatment process and help ensure the long-term success of your root canal therapy. Research has shown that teeth that receive proper final restorations after root canal treatment have significantly higher long-term survival rates than those left with temporary fillings. During these follow-up visits, your dentist will evaluate how the tooth is healing, check for any signs of persistent infection, and ensure that your bite is properly adjusted to prevent excessive pressure on the treated tooth.
Medications for Root Canal Pain Management
Various medications can help manage pain before, during, and after root canal treatment. Understanding your options can help you make informed decisions about pain management. Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) and naproxen (Aleve) are often the first choice for dental pain because they reduce both pain and inflammation. Research has shown that ibuprofen in doses of 400-600mg is particularly effective for dental pain, with 600mg providing better relief in the first 30 minutes. NSAIDs work by inhibiting the production of prostaglandins, which are key mediators in the inflammatory process and pain signaling. This dual action makes them especially valuable for dental pain, which is often inflammatory in nature.
Acetaminophen (Tylenol) is another effective option, especially for patients who cannot take NSAIDs due to medical conditions or medication interactions. While it doesn’t reduce inflammation, it does provide pain relief through different mechanisms. Many dentists recommend alternating between ibuprofen and acetaminophen for more comprehensive pain control. For example, taking 600mg of ibuprofen, then 500mg of acetaminophen three hours later, and continuing to alternate can provide more consistent relief than either medication alone. A landmark study in the Journal of the American Dental Association found that this alternating approach provided superior pain relief compared to opioid medications for dental pain, with fewer side effects.
For more severe pain, your dentist may prescribe stronger medications. These might include prescription-strength NSAIDs or, in some cases, opioid medications for short-term use. However, with proper management of inflammation through NSAIDs and the use of local anesthetics during the procedure, most patients find that over-the-counter medications are sufficient for managing post-root canal discomfort. Always follow your dentist’s recommendations regarding medication dosage and timing, and be sure to inform them of any medications you’re currently taking to avoid potential interactions. After your dental crown placement, similar pain management approaches may be recommended. It’s worth noting that the dental profession has moved toward more conservative use of opioid medications in recent years due to concerns about dependency and side effects, with research supporting the superior efficacy of properly dosed non-opioid alternatives for most dental pain.
Natural Remedies for Root Canal Pain Relief
In addition to conventional medications, several natural remedies can complement your pain management strategy after a root canal. While these shouldn’t replace professional dental care or prescribed medications, they may provide additional relief for some patients. Saltwater rinses are one of the most effective natural remedies for post-root canal discomfort. Mixing half a teaspoon of salt in 8 ounces of warm water creates a solution that can help reduce inflammation, clean the area, and promote healing. Begin these rinses 24 hours after your procedure, gently swishing the solution around your mouth before spitting it out. The hypertonic saline solution works through osmosis to draw out fluid from swollen tissues while creating an environment less hospitable to bacteria.
Clove oil contains eugenol, a natural compound with anesthetic and anti-inflammatory properties. Applying a small amount to a cotton ball and gently placing it near (but not directly on) the affected area may provide temporary numbing relief. Eugenol has been used in dentistry for generations and is actually a component in some dental materials due to its therapeutic properties. Cold compresses applied to the outside of the face can help reduce swelling and temporarily numb the area. Apply for 20 minutes, then remove for 20 minutes, repeating as needed. Some patients also find relief through gentle jaw exercises that help reduce tension and promote blood flow to the area. Simple exercises like slowly opening and closing your mouth or gently moving your jaw from side to side can help prevent stiffness that sometimes develops after keeping your mouth open during dental procedures.
Maintaining proper hydration and nutrition is also important for healing. Drinking plenty of water helps support overall health and can help manage inflammation. Foods rich in anti-inflammatory compounds, such as those containing omega-3 fatty acids (like fatty fish), turmeric, and ginger, may help reduce inflammation throughout the body. However, remember to stick to soft foods that don’t require much chewing while you’re recovering from your dental treatment. Always consult with your dentist before trying natural remedies to ensure they won’t interfere with your treatment or prescribed medications. While natural approaches can be beneficial complementary strategies, they should be viewed as supplements to, rather than replacements for, conventional care. Research in integrative dentistry suggests that a combined approach often provides the best outcomes for patients seeking both effective pain management and minimal medication use.
Long-Term Pain Management for Root Canal Patients
While most patients experience only short-term discomfort after a root canal, a small percentage (approximately 5%) may develop persistent pain lasting six months or longer. Understanding the potential causes and management strategies for long-term pain is important. If you’re experiencing persistent pain after a root canal, it’s essential to consult with your dentist or endodontist. The pain could be due to several factors, including missed canals during the initial treatment, root fractures, infection that wasn’t completely eliminated, or issues with the restoration (filling or crown). Research in endodontic microsurgery has revealed that human teeth often have complex anatomical variations, with some teeth containing accessory canals that may be difficult to detect and treat without specialized equipment.
For some patients, the pain may not be related to the tooth itself but could be due to other conditions such as temporomandibular joint (TMJ) disorders, referred pain from other teeth, or neuropathic pain. Accurate diagnosis is crucial for effective management. This may involve additional imaging such as cone-beam computed tomography (CBCT) scans, which provide detailed 3D images of the tooth and surrounding structures. Your dentist may refer you to an endodontic specialist for evaluation if the cause of the pain isn’t immediately apparent. Endodontists receive an additional 2-3 years of specialized training beyond dental school and have expertise in diagnosing and treating complex cases of dental pain, particularly those involving previously treated teeth.
Treatment options for persistent pain may include retreatment of the root canal, surgical procedures such as apicoectomy (removal of the root tip and surrounding infected tissue), or in some cases, extraction of the tooth and replacement with an implant or bridge. For neuropathic pain, medications that target nerve pain, such as certain antidepressants or anticonvulsants, may be prescribed. Some patients also benefit from alternative approaches such as acupuncture or cognitive behavioral therapy to help manage chronic pain. Remember that persistent pain is relatively uncommon, and most root canal treatments are successful in eliminating pain and saving the natural tooth. A comprehensive study published in the Journal of Endodontics found that even teeth with complex problems and previous failed treatments had a success rate of over 80% when retreated by specialists using modern techniques and equipment. This underscores the importance of seeking specialized care when dealing with persistent pain after endodontic treatment.
Conclusion
Understanding root canal pain management options is essential for anyone facing this common dental procedure. While root canals have long had a reputation for being painful, modern techniques and pain management strategies have made the process much more comfortable than in years past. With proper care before, during, and after treatment, most patients experience minimal discomfort while preserving their natural teeth. The comprehensive approach to pain management, from pre-operative medications to advanced anesthetic techniques and post-operative care, ensures that patients can undergo this tooth-saving procedure with confidence and comfort.
Effective pain management begins before your procedure, with over-the-counter medications and home remedies to address acute symptoms. During the root canal, local anesthesia ensures you remain comfortable, with sedation options available for those with dental anxiety. After treatment, a combination of medications, cold compresses, and dietary modifications can help manage any temporary discomfort as your tooth heals. This multi-faceted approach addresses pain at every stage, significantly improving the patient experience and treatment outcomes.
Remember that communication with your dental team is key to a positive experience. Don’t hesitate to discuss your concerns about pain and ask questions about the pain management options available to you. Your dentist wants you to be comfortable and will work with you to develop a personalized approach to managing discomfort at every stage of treatment.
If you’re experiencing tooth pain or have questions about root canal therapy, we encourage you to contact our endodontic specialists for a consultation. Early intervention is key to preserving your natural teeth and maintaining your oral health for years to come. With the right approach to pain management, you can approach your root canal treatment with confidence, knowing that relief from your dental pain is just around the corner.

 718-979-2121
718-979-2121